What is Bone Marrow Transplantation Hematopoietic progenitors or transplant?
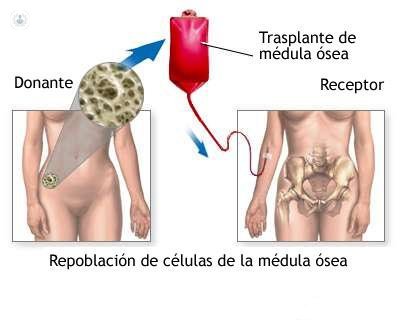
Written by:Transplantation of hematopoietic precursors, known as bone marrow transplantation is the treatment by which a patient 's bone marrow is destroyed, replacing new hematopoietic precursors. Usually performed in patients with cancer or congenital disease of the blood or bone marrow. The aim is to remove diseased or defective cells and introduce stem cells to produce healthy blood cells.
Origin of bone marrow transplantation
The first bone marrow transplant was performed by Georges Mathé, a French oncologist, in 1958, to try to save the lives of six nuclear researchers who had undergone radiation accident at the Vinca Nuclear Institute. Although all patients underwent transplant rejection, Mathé understood the need to improve the procedure of great potential in the field of immunotherapy.After years of research, Mathé managed to improve technique, becoming the pioneer in the use of bone marrow transplantation in leukemia treatment. The transplant was performed using stem cells derived from bone marrow by a team at the Research Center Fred Hutchinson Cancer 1950-1970 E. Donnall Thomas, whose work was later awarded the Nobel Prize for Medicine.
Why bone marrow transplantation is used
Transplantation of bone marrow or purified hematopoietic progenitors is used to treat various types of diseases:- Bone marrow aplasia- Hereditary diseases- Leukemia- Lymphoma- ImmunodeficienciesMany recipients are patients with multiple myeloma or leukemia, who could not benefit from an extended cytostatic treatment, or already have resistance to chemotherapy. They are also candidates those pediatric cases where the patient has a defect serious spinal congenital, such as congenital neutropenia or combined immunodeficiency, with defective stem cells, and children or adults with aplastic anemia who have lost their stem cells at birth.
Other diseases treated with bone marrow transplants include sickle cell anemia, myelodysplastic syndrome, neuroblastoma, lymphoma, Ewing sarcoma, desmoplastic small round tumor cells, chronic granulomatous disease or Hodgkin's disease.Also recently mieloblativo not transplant or "mini transplant" has developed procedures that require fewer doses of chemotherapy and radiation preparative. This has allowed to extend to older patients too weak, along with other patients, considered the therapy to maintain such aggressive treatment.
Types of hematopoietic stem cell transplant or bone marrow
After several weeks of growth in bone marrow, the expansion of hematopoietic stem cells and their progeny is sufficient to normalize blood cell counts and reset the immune system.
Depending on the source of stem cells, we know the following:1) AutologousThis type of procedure uses hematopoietic precursors of the same patient will receive the transplant. As the transplanted cells are taken from bone and damaged, many protocols use some techniques to choose healthy cells to be returned to the patient. This process may require drugs or antibodies designed to remove certain types of cells or marrow purging of neoplastic cells.
To perform this extraction therapy (apheresis) hematopoietic stem cell and the patient is required to store the harvested cells in a freezer. After the patient is treated with high doses of chemotherapy with or without radiation, with the intent to eradicate malignant cells and results in the total or partial ablation of bone marrow (destruction of the capacity of the production of new cells in the bone that is). Later healthy hematopoietic progenitors are returned to the patient's bloodstream, replacing the destroyed tissue and resuming normal production all hematologic series.
Autologous transplantation has the advantage of having a lower risk of developing an infection in the immunocompromised part of treatment, since the recovery of immune function is rapid. In addition, the incidence of patients experiencing rejection is rare, because the donation and reception is the same individual. These advantages have been considered by experts in hematology autologous transplantation as a standard treatment for diseases such as lymphomas. However, for other as acute myeloid leukemia, increasing the likelihood of relapse makes allogenic mode is chosen.
2) AllogeneicThis type of transplant uses hematopoietic precursors taken from a different donor to recipient. This transplant is, in turn, different varieties, depending on the donor and the similarity system Human Leukocyte Antigens (HLA). It is important to recognize what type of transplant is speaking, since both the utility and the results vary from one to the other. When the donor is an identical twin brother is called syngeneic transplant. However, when the donor is a sibling HLA is called allogeneic HLA-identical sibling. In the event that the donor is a family member who shares a single haplotype of the HLA system is called haploidentical transplantation may be a relative anyone (father, mother, brothers, cousins) who share only half of the genes involved in the HLA system. If the donor is an unrelated donor transplant is called unrelated donor.
Transplants involving a donor and recipient are genetically identical not always associated with HLA differences between graft and host. In these cases, the transplanted immune system recognizes as foreign antigens HLA receptor cells and attacks. Therefore it is necessary to select donors maximizing the amount of HLA antigens shared by donor and recipient. HLA antigens are inherited in a Mendelian manner, so often is a family that shares the HLA genes. If there is a compatible related donor can search for unrelated donor HLA compatible yes.
Allogeneic transplants performed using also cord blood as a source of stem cells. In general, by transplanting healthy stem cells of the immune system of the recipient, allogeneic hematopoietic stem cell transplants appear to increase the chances of cure or long-term remission.
Source of hematopoietic progenitors
- Bone marrowThe bone marrow was the first source of stem cells transplanted. As already mentioned, this type of transplant is done with cells taken directly from the donor bone marrow, usually aspirated from the iliac crests through a large needle that reaches the center of the bone. The technique is performed under general anesthesia.
- Peripheral bloodHematopoietic cells can be collected from donor blood using a process called apheresis. Before the transplant, the donor is stimulated by injections of granulocyte colony-stimulating factor (G-CSF) to produce and mobilize more hematopoietic precursors. Obtaining or collecting the donor it is done through a needle placed in a vein in the arm connected to a machine that collects the cells to be transplanted. The remaining blood is returned to the donor.
- Umbilical cord bloodThe cord blood contains stem cells that can be transplanted hematopoietic cell separation after the rest of the tissue (or Lin- CD34 +). Transplants with cord blood not require as much compatibility between donor and recipient. However, the low number of cells in each cord makes the use of a single donor to transplant into an adult or youth is difficult. Sometimes cord blood from two different donors to the number of transplanted cells used is sufficient.It is obtained when a mother donates her baby's umbilical cord and placenta after birth. Cord blood has a higher concentration of hematopoietic progenitors that are circulating in the blood of an adult person. However, the small amount of blood from an umbilical cord (usually 50 ml) makes it suitable for transplantation in young children than in adults. New techniques using ex-vivo units of umbilical cord blood or the use of two cord blood units from different donors expansion, allow this type of transplant can be used in adults.
- ConditioningIn most cases eliminate it needs progenitors already present in the recipient's bone marrow. During this process, called conditioning, high-dose chemotherapy and / or radiotherapy to destroy all the bone marrow of the patient in order to kill cancer cells, prevent graft rejection are used, and leave room for grafting. Common schemes include some drugs.Conditioning leaves the patient without immune and unable to produce red blood system, so you will not die if trasplantase a new bone. Toxic therapies that are used in this process can damage a variety of tissues and are associated with complications such as pulmonary and neurological disorders and a higher risk of cancer in the future.In severe immunodeficiencies, the recipient's immune system is already weak enough for the transplant can be performed without preparation.
- PrendimientoImmediately after transplantation, the transplanted stem cells are housed in the bones and begin to reconstitute the patient's hematopoietic tissues. This process, known as engraftment, is carried out for a few weeks (usually between day 15 and 21) after after implantation. Graft rejection may prevent the ignition and leaving the patient without sufficient hematopoietic function.
Edited by Patricia Crespo Pujante


