Evolution of insemination with donor sperm
Written by:The use of insemination with donor sperm (IAD) was performed for the first time in 1884 in Philadelphia. In addition, in order to avoid sexually transmitted infections (including HIV), cryopreservation prior to insemination was imposed.
However, with the technique of ICSI (intracytoplasmic), which improved semen quality, the indications for IAD declined.
After this breakthrough, there was another: the discovery of the effectiveness of sperm extracted directly from the testicle or epididymis for fertilization of mature oocytes.
Even so, insemination donor sperm are still the procedure of choice for Assisted Reproduction in many patients. In fact, in recent years the total number of cycles IAD has increased (especially as a result of more women without a male partner who wants to be mother).
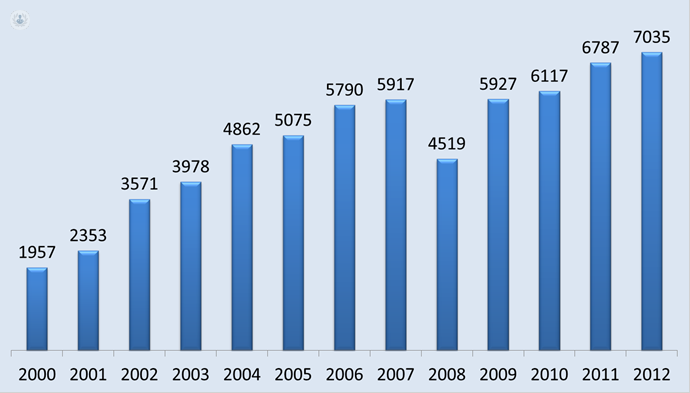
Total number of cycles graphically IAD from 2000 to 2010 published in the National Register of the Spanish Fertility Society
Frozen semen quality
What is clear is that the use of frozen semen gets lower pregnancy rates than fresh semen, although they have created different strategies to increase the pregnancy rate.
Pregnancy rate of IAD
According to data published by the Register of the Spanish Fertility Society based on 7,035 cycles performed in 2012, the pregnancy rate of IAD is 20% per cycle. This percentage depends on the following factors:
- Semen cryopreservation. He appeared in the 90s with the emergence of human immunodeficiency virus (HIV), in order to avoid. In addition, cryopreservation facilitates the fact of anonymity between donor and recipient woman. To carry out the process is necessary to consider sperm dilution, refrigeration and freezing and thawing speeds (the critical temperature range for sperm to survive during freezing is between -10 and -40 degrees Celsius).
- Effects of cryopreservation of sperm function. The most decisive effect that freezing has on sperm is loss of mobility.
- Semen quality. In general, the appropriate number of motile sperm for IAD cycle has to be at least 5 million. Most sperm banks reject donors in more than 20 million motile sperm per milliliter is not recovered after thawing.
- female diagnostic. It is essential to make women a study prior to insemination fertility, as the use of donor sperm does not solve possible factors of female infertility.
- Type insemination. Intracervical IAD is less effective than intrauterine IAD. The latter requires prior sperm capacitation in which potential factors that could reduce fertility are eliminated.
- ovarian stimulation. Most published works agree that the pregnancy rate in IAD is higher in stimulated cycles in spontaneous cycles. Although the most aggressive ovarian stimulation may increase pregnancy rates, it also increases the risk of multiple pregnancy (the average pregnancy rate per cycle is 29%, 10% of which of gemerales pregnancies).
- Number of inseminations per cycle.
- Number of cycles of insemination. The work carried agree that most pregnancies were achieved in the first four cycles (84%). In fact, we do not recommend more than 4 insemination cycles with donor sperm.
Ethics insemination with donor sperm
One of the controversial points in the insemination with donor sperm is the revelation of the origins of the child born through these techniques. There are several rights that can not be simultaneously respected:
- The right to autonomy and privacy of patients.
- The right to privacy of donors.
- The right of the child to know its origins.
In Spain, it is mandatory to respect the anonymity of the donor.



