Dry eye: symptoms and causes of dry eye
Written by: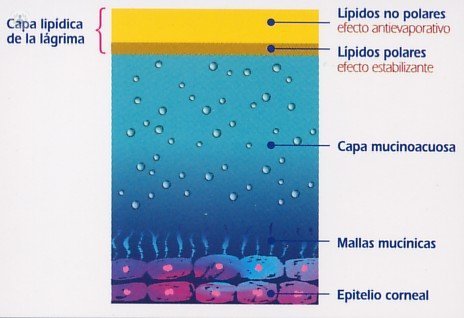 Dry eye is defined as the heterogeneous group of diseases in which the tear film, for qualitative or quantitative alterations, fails to maintain adequate moisture ocular surface. It manifests as the subjective sensation of dryness or lack of tear, causing various symptoms of ocular discomfort such as rubbing, itching, burning, grittiness, blurred vision, burning or lack of lubrication.
Dry eye is defined as the heterogeneous group of diseases in which the tear film, for qualitative or quantitative alterations, fails to maintain adequate moisture ocular surface. It manifests as the subjective sensation of dryness or lack of tear, causing various symptoms of ocular discomfort such as rubbing, itching, burning, grittiness, blurred vision, burning or lack of lubrication.
Today is known to be the most common problem in ophthalmology , but fortunately only rarely becomes very serious. What mainly suffered by women after menopause, due to horonales changes, while also occurs with advancing age, systemic enfermedaades and drug treatments, but really anyone can be affected.
Types of Dry Eye
Any diagnosis of dry eye should be defined by three parameters:
- Cause
- Histopathology: the type of dacrioglándula affected
- Gravity
Causes Dry Eye
Causes of dry eye can be combined into 10 groups, in which the first 5 usually affect many exocrine glands (eyes, nose, mouth, vagina, skin), while the last 5 usually affect only the glands of both eyes, one eye, or even a single glandular variety of an eye:
- Age Origin: With age everyone just having a pan-exocrine sicca, which affects the eyes, mouth, throat, etc.. The age dry eye is usually mild or medium (grade 1 or 2).
- Hormonal origin: If testosterone decreases or do not have enough testosterone receptors, the gland begins to hipofuncionar. Since women have very few androgens, when menopause arrives and decreases androgen status can begin to develop dry eye. Therefore: castration, aging, hipoovarismo, antiandrogen treatment, oophorectomy, postmenopausal, estrogen contraceptives and breast-feeding are situations in which tear secretion decreases and mild dry eye occurs.
- Pharmacological Origin: There are multiple drugs that can cause eye dryness hyposecretory side - effects have exocrine: anxiolytics, antidepressants, sleeping pills and hypnotics, antiparkinsonian agents, antihistamines, anticholinergics, arterial antihypertensives, diuretics, etc.
- With immunological or immunological origin: We can distinguish two groups: autoimmune processes exocrine glands or Sjögren's syndrome and immune processes not exocrine tissues, but including the glands, affecting them. Some infectious diseases, such as infection with the Epstein -Bar, seem to favor the autoimmune attack against the exocrine glands.
- Hiponutricional Origin: Dry eye by malnutrition or vitamin deficiency was the most common cause of severe dry eye for millennia, and continues to do so in developing countries. In developed countries they are rare, and usually caused by intestinal malabsorption (alcoholism, Crohn's disease, bowel resections, etc.) or fat-free diets. Other deficits that may present with dry eye are: severe degrees of water dehydration, vitamin deficiency B2, B12 vitamin deficiency and iron deficiency and potassium depletion.
- Glandular dysgenesis: They are due to embryo-fetal malformations, which may have a genetic origin or occasional. In the first case can be hereditary and the second not. They can affect many exocrine systems, or only to tear one or both eyes, or even just one of 3 sub glandular eye.
- Inflammatory origin: Inflammation, usually infectious, of the lacrimal glands, affecting aqueous glands, affecting the mucous membrane lining the eyeball.
- Traumatic origin (destructions by physical or chemical agents): The destruction of the glands can cause eye dryness. The severity of traumatic dry eye is highly variable depending on the involvement of trauma. Sometimes it can acquire serious cases.
- Neurodeprivativo origin: lacrimal secretion has nerve stimulation can be altered in cases of facial paralysis or nerve damage. Similarly, fatigue, sleepiness and anxiety also decreased lacrimal secretion. Restricted REM sleep reduces the already low secretion during sleep.
- Tantalic eyes: Tantalic eyes are those that still have normal or even excessive lacrimation, ocular surface can not take advantage. Dry eyes are those having a normal lacrimal production can not exploit the cornea is tear, either by disorders of the epithelium cause the slide on the cornea tear or because the lids can not be adequately extend tear on the corneal surface.
histopathologic classification
Dry eye can also be classified according to the lacrimal gland is affected:
Often dry eye is due to dysfunction of the three types of dacryoglands forming the lacrimal: aqueous, mucous membranes and lipid. It can affect one of three subsystems, two or three, and although initially affected is only one, in the course of the disease often secondarily affected all.
Most dry eyes are included in diseases that affect many exocrine glands:
- Nose: dryness, itching, anosmia.
- Mouth thirst, thick saliva, expelling sputtered, altered taste and halitosis or bad breath.
- Throat: thirst, hoarseness, phlegm and dysphonia.
- Vagina: itching, painful intercourse.
- Seminal glands: dense sperm.
- Skin: dryness, itching.
- Ear wax plugs and itching of the ear canal.
Often dryness suffering from a gland does not correspond to the feeling that the patient has: usually elderly often feel discomfort in the eyes, and then in the mouth. Dry throat, nose and vagina, usually occupy an average degree. While dry skin ear and usually go unnoticed frequently.
Classification clinical severity of dry eye
The severity of dry eye is expressed in 5 degrees: subclinical, mild, medium or moderate, severe and disabling.
- Subclinical or minus grade 1: The patient has a dry eye in its infancy, but only experience symptoms of dryness in situations of overexposure (use of contact lenses, exposure to wind, fan, air conditioning, etc.). At this level the patient normally not known to have ocular dryness. Symptoms that are transiently feel: sensation of dryness, grittiness, eye fatigue and blurred vision that disappears when you blink. Usually in this degree the patient is unaware that already has dry eye.
- Grade 1 or Mild: The patient often notice symptoms of dryness and itching, photophobia or fatigue, even in normal environmental conditions. Often at this stage the dry eye patient confused with other diseases such as conjunctivitis, infections or allergies.
- Grade 2 or Moderate: A reversible signs the above symptoms which are characterized by the presence of lesions of the ocular surface, as epithelial erosion, punctate keratopathy, conjunctival hyperemia of trigoni or crusting added. It is diagnosable signs with the slit lamp. new subjective symptoms of dry eye, such as difficulty in opening eyes to wake up in the morning, tingling or burning also appear.
- Grade 3 or Grave: They appear permanent or irreversible signs due to the dryness of the ocular surface: corneal hypoesthesia, ulceration and litchis of the corneal stroma, walleye, squamous metaplasia of the ocular surface, corneal neovascularization, conjunctival scarring, retraction of lacunar grooves ( between the nasal conjunctival fornix and plica lunate, and the lunate between plica and caruncle). These lesions persist and worsen if the box dry eye progresses, and not totally disappear if the lacrimal drainage improvement.
- Grade 3 or incapacitating plus: Damage to the cornea causes a loss of more or less severe vision: central disabling corneal ulcers, central corneal scars, corneal epithelial keratinization.
Dry Eye Treatment
There are many treatments, but usually not curative since in most cases the etiology can not be treated the same, and the disease usually persists for life.
Treatments that improve the quality of life of patients with dry eye can range from health and environmental measures, to etiological treatments when possible, and substitutes lagrima, drugs to stimulate tear secretion, mucosecretores and mucolytics, immunosuppressants, or cases that surgical and regenerative agents or serum enriched plaquetes techniques are necessary.
Dry Eye Prevention
To delay the most eye sequedat and that affects the eye as little as possible, with environmental media, adequate food and avoiding certain medications and situations whenever possible.


