10 questions on retinopathy and diabetic macular edema
Written by:
Diabetes has become one of the most serious health problems worldwide. An estimated 55% increase in people with diabetes by 2035, from 382 million patients in 2013 to 592,000,000 in 2035 patients.
It is estimated that 8.3% of adults have diabetes, of which 35% diabetic retinopathy (DR) and 7% diabetic macular edema (DME). In Spain it is estimated that 13.8% of the population is affected by diabetes, which know their situation about half of them.
What is the relationship duration of diabetes with these diseases?
At 20 years of onset of diabetes, almost all patients with type 1 diabetes have some degree of RD, reaching 60% in patients with type 2 diabetes.
EMD prevalence differs depending on the type of diabetes and treatment based on: type 1 (11.5%) diabetes; type 2 diabetes treated with insulin (9.1%) and type 2 diabetes not treated with insulin (4.1%). The cumulative incidence at 25 years of evolution of diabetes is 29%.
What are the risk factors for diabetic macular edema appearance?
There are three main systemic factors:
- Systolic blood pressure high
- Total cholesterol elevated serum
- High levels of glycosylated hemoglobin (HbA1c)
How to view the DR and DME affects?
Diabetic retinopathy occurs in the beginning, a change in vascular permeability of the blood vessels of the retina which causes the output of components of blood plasma into the retina (diabetic retinopathy). The liquid inside the central part of the retina, the macula, is what produces the diabetic macular edema, which is the main cause of vision loss in patients with diabetes.
What are the early symptoms?
Initially it may not show anything, but the most common symptoms are:
- Decreased visual acuity
- The presence of spots in vision that limit us vision
When the detection of diabetic retinopathy and diabetic macular edema done?
Both the RD and the EMD may go unnoticed in early stages of disease. This situation makes early detection is critical to obtain the best visual results.
Start screening:
- Type 1 diabetes within five years of diagnosis of diabetes or in patients over 10 years.
- Diabetes type 2: at the time of diagnosis or as close to it.
Frequency of screening:
- Every year in type 1 diabetes
- Every two years in patients with type 2 diabetes without signs of RD, in the case of metabolic control is good and the disease is short evolution
- Each year in patients with type 2 diabetes without signs of RD, in the case of poor metabolic control or more than ten years of evolution
How detection of diabetic retinopathy and diabetic macular edema done?
Although there are screening programs for diabetic retinopathy, based on fundus photographs in primary care centers, detection and ideal monitoring it is the complete eye examination by a study of the fundus under pupillary dilation. During it is performed: making visual acuity, intraocular pressure measurement and detailed examination of the anterior and posterior segment of the eye.
What are the additional tests are needed for diagnosis and follow - up?
No test replaces the complete eye examination performed by an ophthalmologist. The usual complementary tests are:
- Retinography: involves the taking of a photograph of the fundus. According to the available system you can be done with or without dilated. It allows us to document the evolution of the DR and DME (Figure 1).
- Fluorescein Angiography is a photograph of the fundus, which is performed after application of intravenous contrast through the patient's arm. It is not used for diagnosis, but for cases or if required for carrying out treatments such as laser (Figure 2).
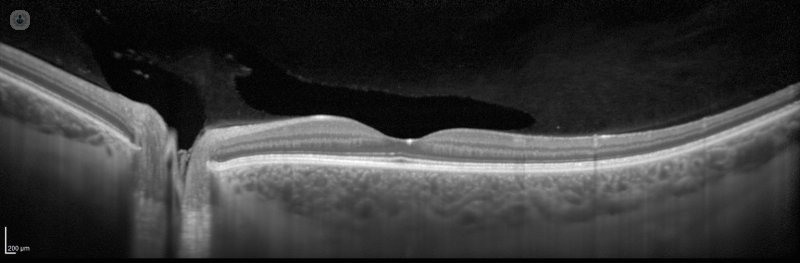
- Optical coherence tomography (OCT) is a type of laser eye scan, during which can be studied at the microscopic level, the different structures that form the retina and measure the degree of macular edema. It has become the essential test for optimal monitoring of patients with macular edema and compulsory in the event that you are being treated for the same. It is done in seconds, it has no side effects and can be performed as often as necessary (Figure 3).
Which is the treatment?
The main treatment is to control diabetes, either by the primary care physician as endocrine. This will help control the evolution and better treatment effect.
From the point of view ocular, currently available treatments are:
- Intravitreal injections of anti-VEGF drugs: are made with the application of anesthetic drops and is done in a few seconds, almost without noticing anything. They can carry out those necessary, but between them must pass at least one month. They are indicated when there are diabetic macular edema and the method has shown better results in maintaining and improving vision.
- Injection of intravitreal steroids: an intraocular device that releases corticosteroids injected progressively. Its effect lasts about 4-5 months and sometimes it is necessary to inject different times over the course of the disease.
- Laser photocoagulation of the retina being a destructive treatment, its use is shrinking. However, in cases of proliferative diabetic retinopathy and a particular type of macular edema still they have their indication.
- Vitreoretinal Surgery: only indicated in very advanced cases of proliferative diabetic retinopathy and diabetic macular edema with tensile component.
The person who guides the treatment or combination of treatments to follow is the specialist ophthalmologist retina.
If I have diabetic retinopathy or diabetic macular edema I'll stay blind?
Today the available treatments assure us that a person control their acceptable diabetes, with RD and / or EMD is detected early and will perform checks and timely treatment, over time you need, not run blind.
1. Retinography image of both eyes of a patient with diabetic retinopathy and diabetic macular edema, which lesions lipid exudates as diabetic retinopathy (marillas spots) and bleeding (red spots) were observed.
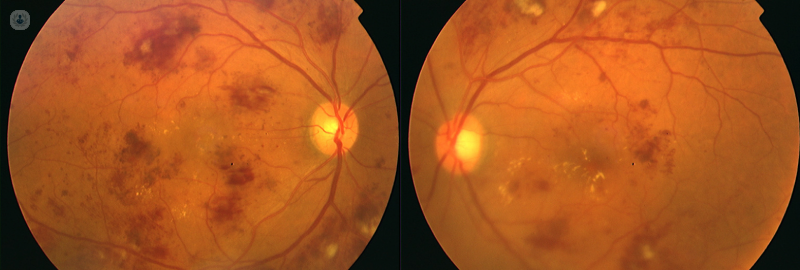
Image 2. Fluorescein angiography image of wide field, which can be seen proliferative diabetic retinopathy has been treated with laser photocoagulation of the retina (white dotted seen in the image)
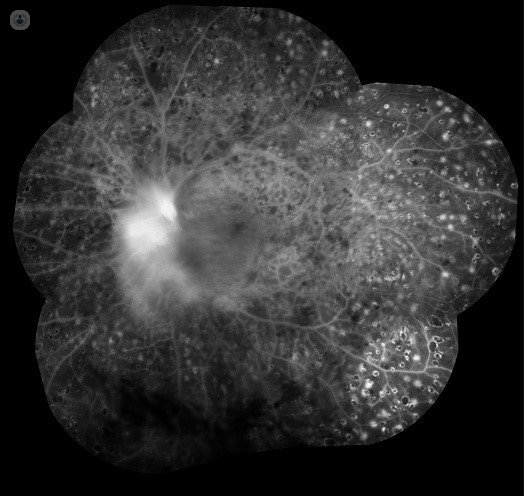
Figure 3. Image of optical coherence tomography, wide field, from a healthy person.