Qué es y cómo se trata la membrana epirretiniana macular
Written by:The doctor. Bueno Palacín, expert in the diagnosis of any pathology related to the retina, is the director of the Vitreo-Retina Unit of Innova Ocular IOA MADRID. In the following article he explains what is and how the epiretinal membrane is treated.
The macula is the central area of the retina, which occupies a few millimeters of the same. It directly affects the light rays that penetrate the eye, so it is the area that gets a better view. This area allows us to identify fine details, read, thread a needle or recognize faces, among others.
The peripheral retina serves to expand the visual field, helping spatial orientation. This allows us to know what we have on our right and what is on our left, but not precisely. For example, if we have our eyes fixed to the TV we can see that there are furniture on their sides, but if we put a text next to the TV we can not read it. This is because the peripheral retina does not have detailed vision capability.
The epiretinal membrane or epimacular membrane is a thin layer of fibrous tissue that grows on the surface of the macula.. Over time, this membrane tends to shrink little by little and causes a progressive deformation of this central area of the retina.

What causes the appearance of the epiretinal membrane?
Most of the time, the appearance of the epiretinal membrane does not have a definite cause but it is related to the age of the patient. Normally it is rare to see an epiretinal membrane below 50 years of age, being diagnosed more frequently in the 70s.
A small percentage of these epiretinal membranes may have an inflammatory origin, arising as a reaction to trauma, surgery, intraocular inflammation, laser treatment or in relation to vascular or tumor diseases.. This type of epiretinal membranes can occur at any age.
What are the symptoms of the epiretinal membrane?
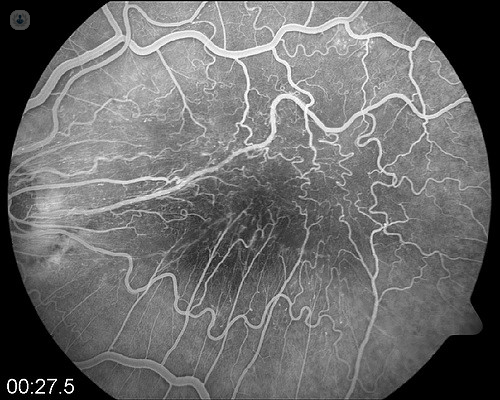
When the membrane is recent, it is slightly contracted and deforms the macula a little, so it may not have any symptoms. The patient can maintain good vision and, as the membrane is so thin, it can even go unnoticed by the doctor in a routine fundus examination. We have a device known as OCT, which performs a small scan of the macula and is very sensitive to detect the presence of these membranes even in these early stages.
As the membrane contracts, the deformation of the macula is increasing and the symptoms it produces are mainly two:
- The first and most important is the decrease in central vision. This is easy to identify in a scan because the affected eye, even if it is well graduated, is able to see fewer letters than the healthy eye when a visual acuity test is done.
- The second is the appearance of metamorphopsia, which is the appearance of deformity in vision. This the patient refers to it saying that by an eye he sees the crooked objects, if he compares it with the good eye.
Can the epiretinal membrane be prevented?
The epiretinal membrane can be attempted only when its origin is inflammatory, and can be prevented with treatment. In the vast majority, the membrane usually arises spontaneously, so it can not be prevented.
How is the epiretinal membrane treated?
Currently there are devices that help in the early diagnosis of these membranes. Many of them do not need to be treated since they do not cause great visual alterations and the treatment can be limited to a follow-up. In addition, its evolution is usually very slow and with an annual review, or two, it is usually enough to have them under control.
When these membranes clearly affect the visual acuity of the patient, either due to loss of vision or because the distortion they cause is large, the only solution is to perform an intervention called posterior vitrectomy.. This intervention consists, basically, in entering the eye and eliminating a gelatinous liquid inside, known as vitreous, in order to access the macula.. Once there is free access to the macula, a dye is used that dyes the blue membrane and allows better identification. Then, with very small forceps, we try to separate the membrane from the macula little by little to remove it without damaging the underlying retina.
If we have a macula deformed by the existence of a membrane on its surface and successfully remove that membrane, what is intended is to stop the process of progressive deformity of the macula and, at least, stop the loss of vision. In addition, once the macula of the traction has been released, we increase the possibility that the macula tends to recover its habitual shape and improves vision and distortion.
In general, the results are better in patients who have not lost much vision before being operated on. This is logical, because if a patient has a severe visual impairment means that the membrane has long evolution, with a macula deformed for a long time and, therefore, with less ability to recover its original shape and improve vision. There is no fixed rule of when an epiretinal membrane should be operated, nor a limit of loss of vision from which it must necessarily operate. In spite of this, as a general rule, it is necessary to know that the better the vision before operating, the greater the possibility that the visual recovery will be good and vice versa. If we observe that in successive revisions the patient remains stable, it would not be necessary to do anything, but if his vision loss is progressive, it would not be advisable to wait a long time to operate.


