El desprendimiento de retina: qué es, cómo se manifiesta y cómo tratarlo
Written by:Retinal detachment consists of the separation of the innermost layer that forms the eye and processes the vision, the retina, which moves into the vitreous humor and produces a loss of vision.
What is the retina and what are its parts
The retina is a set of nerve cells arranged in the innermost layer of the eye, whose mission is to transform light stimuli into nerve signals for the brain to interpret. The macula is an area of the retina that captures the central vision, allowing us to focus our attention on details, see closely, read. The rest of the retina is responsible for peripheral vision. The vitreous humor is a gel that fills the eyeball and is in contact with the retina. With the aging or by some illness, the vitreous humor liquefies, forming lumps in the gel.
Types of retinal detachment
As various ophthalmologists report , the more frequent retinal detachment is caused by a tear or hole in the retina, allowing the liquid inside the eyeball to be inserted through these breaks and to separate the retina from the underlying tissue, favoring retinal detachment .
The detachment can also occur by traction. This is less frequent and usually affects diabetics, forming membranes that pull from the retina towards the vitreous.
Serous retinal detachment is more rare and is caused by inflammation of the external layers of the retina that produce fluid that accumulates below the retina and detaches. Myopia, diabetic retinopathy, ocular trauma, the presence of retinal holes, and complicated cataract surgery may also predispose to retinal detachment.
What are the symptoms of retinal detachment?
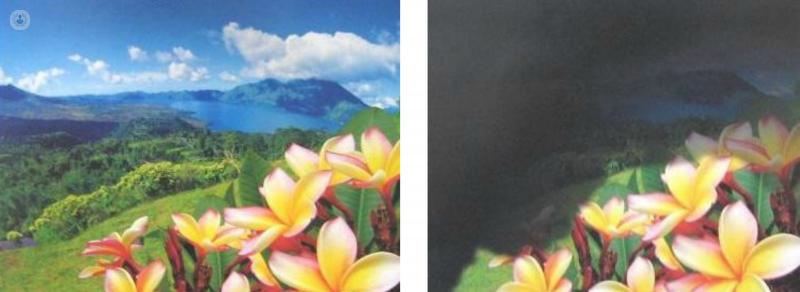
The symptoms are loss of vision, vision of a cloth or a shadow that may appear without warning, although the usual thing to notice is the presence of flying flies or flashes.
Flying flies are points that move in the visual field and are usually unimportant. They are usually due to the aging of the vitreous humor that can cause a posterior vitreous detachment that is an area of this that is separated from the retina and must be controlled. If glare is observed it indicates traction of the vitreous on the retina.
How Retinal detachment is treated and treated
Retinal detachment is not seen by simple observation of the eye. If any of these symptoms are detected, an ophthalmologist should be used to perform an eye exam that determines the size, location, and degree of evolution of retinal detachment.
The treatment of retinal detachment is aimed at restoring the normal position of the retina, which is why surgery is used in many cases. In tears and holes without detachment the laser is used to surround them and prevent it from occurring.
- Injuries to the retina are treated by laser photocoagulation , a technique that is generally painless but can be annoying in a timely manner and is done on an outpatient basis.
- In cases of superior and small retinal detachment can be treated with an injection of gas and then laser around the detachment.
- When the lesions can not be treated with a laser, surgery will be necessary, which may be extra-scleral , placing implants that push around the eyeball and draining the liquid that causes the retina to be detached. In most cases vitrectomy surgery is performed within the eyeball and is intended for anatomic reapplication of the retina. In spite of the treatment, a total recovery of the vision is sometimes not possible although the anatomy of the retina is restored.
The process of surgery on retinal detachment
Before the surgery, it is necessary to perform tests and preparations in order to avoid unforeseen situations that may cause complications in the results. Days before surgery the eye will be checked to assess the state of the retina and in case of cataract, the eye will be operated on in the same procedure.
Vitrectomy surgery is performed under retrobulbar anesthesia assisted with sedation, anesthetizing only the intervened eye. It can also be performed under general anesthesia to keep the patient completely asleep throughout the procedure.
Before starting the surgery the area of the eye is cleansed with an antiseptic solution and kept open with a blepharostat. The first step is to make 3 entries in the sclera, about 3 mm from the cornea, where the instruments will be inserted.
During surgery, depending on the case, to reapply the retina and drain the fluid under the retina you can use perfluorocarbon. Once the retina is applied, membranes can be removed on the retina, using laser or cryotherapy to seal it.
In some cases surgery can be performed or the vitrectomy can be combined with the placement of a silicone band around the eyeball at the same surgical event. Silicone oil is the liquid that keeps the retina in place after surgery, in some cases it can remain inside the eye for a long time, since it is usually extracted after six months. When the silicone oil is removed, the retina can re-detach, so if it is believed that there is a high risk of it happening, it can be left inside the eye, although in the long term it can cause complications such as corneal opacity and glaucoma.
After the intervention, the entries are closed with or without stitches, and anti-inflammatory and antibiotic treatment can be given around the eye, leaving it covered. In the first moments after surgery the vision is very poor .
Post-surgery care for retinal detachment
Typically, discharge is done after the patient has tolerated mouth feeding. An operated patient should not drive or leave the center alone. As soon as the patient may have to face down so that the gas that expands and is holding the retina. In addition, this posture removes the gas from the lens, since it promotes the appearance of cataracts, in cases in which the patient is not operated on.
For several days after surgery, antibiotic and anti-inflammatory eye drops are used, which can be administered one after the other, waiting at least 5 minutes between them. During this time the rest must be maintained strictly and follow the indicated treatment. The average recovery period ranges from one to three months, and by six months the results can be evaluated.


