¿Qué son las Neoplasias Mieloproliferativas y como se diagnostican?
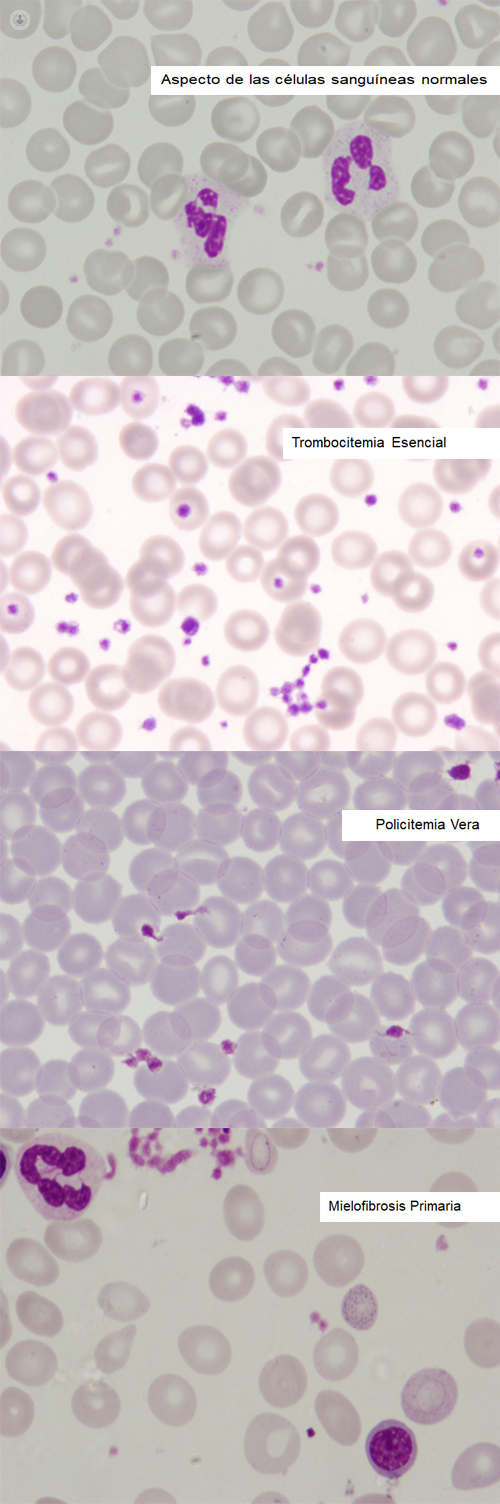
Written by:Myeloproliferative Neoplasms are called a group of three diseases: Essential Thrombocythemia, Polycythemia Vera and Primary Myelofibrosis, which have similar characteristics.
These are chronic diseases that are characterized by an excess production of red blood cells (red blood cells), white blood cells (leukocytes) and platelets (cellular fragments essential for coagulation) that originate in a blood mother cell located in the bone marrow that acquires abnormal behavior (usually due to a genetic mutation that it acquires), starting to proliferate without control.
In a simple way, Essential Thrombocythemia is characterized by an increase in the platelet count, Polycythemia Vera by an increase in red blood cells and Primary Myelofibrosis by a fibrosis (healing) of the bone marrow that is usually accompanied by an increase in platelets. and of the leukocytes in the early stages, but which frequently occurs with anemia and enlargement of the spleen ( splenomegaly ) at the time of diagnosis.
Diagnosis of Myeloproliferative Neoplasms
In general, these diseases are diagnosed in a patient without symptoms, when a routine analysis is performed or for other medical reasons and then an increase of red blood cells, leukocytes or platelets is detected in the case of Essential Thrombocythemia or Polycythemia Vera, or anemia with increased spleen size in the case of Primary Myelofibrosis.
The first step of the hematologist is to differentiate these increases of abnormal cells from the secondary or reactive increases of normal blood cells for other reasons. A patient with a chronic respiratory disease, such as emphysema, or even a smoker may have an increase in red blood cells as a physiological compensation of the organism to a lack of oxygen in the tissues derived from a chronic lung disease or smoking. Another example would be the increase in the number of platelets that can be observed as a reactive phenomenon to the lack of iron in a woman with heavy menstruation and in other circumstances as chronic inflammatory diseases (arthritis).. Likewise, excess leukocytes are relatively frequent in bacterial infections, in smoking or in patients taking corticosteroids.. Therefore, in the first visit, the specialist will try to discover if there is any of these causes that, without being malignant, can produce increases in the number of blood cells.
If a cause that explains this increase is not evident, hematologists should request some tests to rule out or confirm the existence of any of these diseases. As a practical attitude, first ask the patient if he has previous analyzes in which we can see if there was already this increase or a trend to the same. If the previous analyzes were normal and it has been in the last ones in which the increase in maintained form has been documented, we suspect that it could be the beginning of a myeloproliferative neoplasm.
The first step that is carried out is a blood test to detect the existence of mutations associated with these diseases and corresponding to genes called JAK2, Calreticulina (CALR) and thrombopoietin receptor (MPL).
As basic information it should be known that the JAK2 gene mutation, specifically JAK2 V617F is detected in 95%, 60% and 60% of patients with Policitemia Vera, Essential Thrombocythemia and Primary Myelofibrosis, respectively. In case the detection of the JAK2 V617F mutation is negative, the study of the rest of the mutations is requested if we suspect that the patient may have an Essential Thrombocythemia or a Primary Myelofibrosis. The presence of any of these mutations does not mean that they are transmitted in a hereditary way, but that the blood stem cells acquire them for unknown reasons at some point in the patient's life.
When the result of the genetic analysis confirms the existence of any of these mutations, we must request more tests in order to establish a diagnosis of certainty. The main test used for diagnosis is usually the study of the bone marrow through what we call bone marrow aspiration and bone biopsy.. Both tests consist of puncture with a fine needle of an accessible bone area (generally in the iliac crest or in the sternum and local anesthesia) in order to extract a small amount of blood stem cells.. The microscopic analysis of the characteristics and the percentage of these cells will help us to establish a specific diagnosis.
Frequently, an abdominal ultrasound is also requested to detect if the spleen is enlarged, a relatively frequent circumstance, although in a variable percentage, in each of these diseases. With all these data, hematologists apply a series of diagnostic criteria defined by the International Classification of Tumors of the World Health Organization that allows us to confirm the existence of the disease.


