The ongoing debate on PSA: Advantages and disadvantages
Written by:The recommendation to perform PSA (prostate-specific antigen) to all men older than 50 years for screening or early detection of prostate cancer is being increasingly questioned. This marker, which has been used for more than 20 years in clinical practice, has become a routine analytic in the consultations of family doctors and urologists. However, despite its generalization, the recent appearance of several publications, the most recent of the US Preventive Services Task Force (USPSTF) , reopens the debate on its use.
Why to make an early diagnosis of prostate cancer?
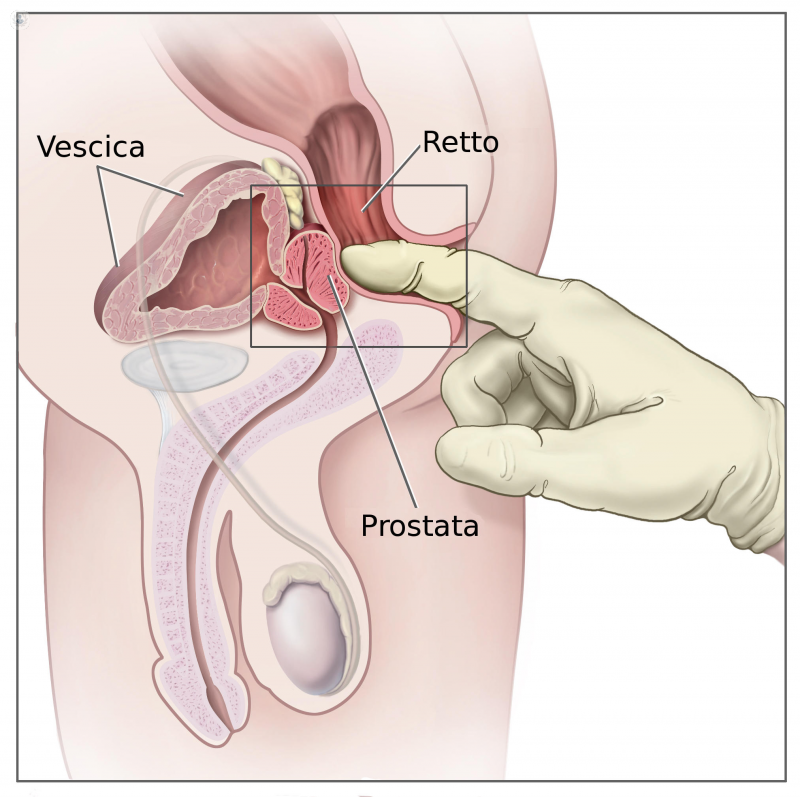
There are a number of reasons in favor of early diagnosis. Undoubtedly, the most significant is that prostate cancer is the most frequent tumor in man, and that early treatment of the tumor increases survival. As noted, 9% of men over 50 years will suffer from prostate cancer (CaP), but only 3% will die as a result of it. To detect it early, a rectal examination is recommended, especially the PSA.. Before the PSA era, only 30% of the tumors were diagnosed at an early stage, that is, they were localized and potentially curable tumors. Since the introduction of PSA, these percentages have changed radically, and now most tumors are diagnosed when they are localized.
The counterpart is that many patients undergo unnecessary prostate biopsies without even having a tumor, and of those who have it, 50% have no clinical relevance, that is, they are overdiagnosed and over treated.. This supposes the probability of secondary effects as a consequence of the treatment, especially two; impotence and incontinence, in a considerable percentage of patients with a tumor with a good prognosis from which they will not die are treated or not. Therefore, the main disadvantages of PSA are that it is not a specific marker of prostate cancer, and that it does not allow the differentiation of tumors that are aggressive, that can risk the patient's life, of those that are not.
Does CaP mortality decrease the PSA quantification?
Despite the wide use of PSA and the countless publications in the scientific literature, we did not have direct evidence to prove the early diagnosis of prostate cancer.. For this, long-term examinations (longer than a decade of follow-up) with a large number of patients were necessary, in which mortality by PCa was compared in patients who had undergone screening or early diagnosis versus patients not submitted (group control). In 2009 two studies were published, one American ( PLCO ) with about 80,000 patients and another European ( ERSPC) that covered more than 150,000, which sought to answer this question. However, the results have not definitively clarified the situation.
In this way, the American study found no differences in survival between the two groups, although as a criticism, 40% of the patients in the control group were subjected at some point to PSA determinations, so this "contamination bias" questions the authenticity of the results. The European study, with more patients, does indicate, at 9 years of follow-up, a decrease in the risk of dying from PCa of 20%. However, to prevent a death by CaP, it was necessary to test 1,410 males and diagnose and treat 48. As an example, in breast cancer, to prevent a death it is essential to test 1,000 women and diagnose and treat 10. With more years of follow-up, recently published results are better, especially in a group of Swedish patients, which further supports the reasoning of those in favor of early diagnosis.
Why continue using the PSA?
In spite of the doubts, the PSA continues being the most effective test that exists to detect the cancer of prostate and for its follow-up when already it has been diagnosed. The key is in its rational use, in how and to whom to request it, and in an appropriate interpretation of its values. Its generalization has led to systematically determining all men who come to a consultation, regardless of their age and without specifying the dangers and benefits of such analysis.. The ideal is to explain to the patient the objectives of its quantification, with its pros and cons and, if it is determined, to rationalize its use. In this way, for example, it should not be done or should not be determined in men older than 70 or 75 years, or in any case in patients with a life expectancy of less than 10 years, since in these cases the advantages of detecting a tumor are few.
It is also not necessary in many cases to quantify it every year, given that in patients who have values less than one, the risk of developing a tumor is practically nil.. Therefore, while waiting for a marker or better test to appear, the PSA will continue to be used, the key is to do it well.



