Dry Eye Treatments
Written by:In most cases the Dry Eye has no definitive treatment and will persist for life. When it is, the patient should be informed by the ophthalmologist and help you accept it : this is not unusual and patients with diabetes or hypertension are also facing a disease that will lead to the end of their lives, is a common occurrence, possible and sobrellevable.
Although not a definitive treatment in all cases, yes there are treatments that can and should follow the patient's dry eye:
Environmental treatment for dry eye
In most cases the etiological treatment is not possible, either because the exact underlying cause of dry eye is not known, or because the cause is unknown but it has no effective medical treatment. For the patient with dry eye symptoms it is recommended to avoid taking steps in their everyday lives, such as avoiding drafts, environmental dryness and pollution:
Air currents favor evaporation of the tear, so that worsen symptoms. It should be noted that strong air currents are picked up by the sensory system of the skin but light streams go unnoticed, such as air conditioners or hot air furnace. Some measures that can be taken are:
- Do not direct fans to face.
- Use heating with radiators rather than air conditioning.
- Do not drive with open windows.
- Wear goggles to avoid direct air against the eye.
Avoid environmental dryness: to not produce symptoms of dry eye, ideally a 35-45% humidity. In the rooms with air conditioning, airplanes (5-15%) and in most kitchens the air has a much lower degree of humidity recommended, causing dry eye.
The main measures to prevent environmental dryness are:
- Avoid dry environments or wet environment, whether commercial humidifiers or by placing a bowl of water on hot areas like radiators.
- Create eye microclimates by normal or sealed goggles. Wearing glasses eye reduces evaporation and protects from drafts.
Prevent environmental pollution: patients with dry eye, having fewer tears have more difficulty to remove dust particles that can enter the eye and under normal conditions they would be washed away and eliminated by the tear. These particles will be retained on the ocular surface and irritated, so the patient should avoid dusty environments such as beach and countryside when it is windy or house dust when lifted when cleaning.
Other substances such as snuff smoke and paint solvents, have components capable of decreasing the stability of the tear film.
As habits, exposure to computers, TV screens and night reading promote tear evaporation due to less frequent flash rate. On the contrary, volunteers are recommended to moisten the eye blinks.
Tips to avoid or reduce dry eye: eye treatment
- forced Flicker forced flashing must be repeated several times a day to expel the contents of sebum to the free edge of the eye lid.
- A massage on the eyelids increases the release of acuoseroso, mucin and lipid components of the tear: it is recommended to massage the upper and lower eyelids with fingers several times a day, on rising, at bedtime and before activities like entering sites air conditioning, air currents, spend several hours at a computer, watching TV or movies, etc.
- Apply warm compresses to the eyelids is useful and can be to wake up in the morning, and if the clinical situation warrants, repeat once or twice during the day. It can also be done as a pre-step massage, enhancing their effectiveness.
- The cleaning is done glands in the eyelid margins that are the greasy surface of the whole organism. Must take special care with soaps that are used, as the inevitable entry of goods into the sea lacrimal causes eye irritation and destruction of the lipid layer.
- Therapeutic use contact lenses: wear contact lenses dry eye is not advisable, since in fact they are one of the causes of it. But you can carry out is the occasional use of highly hydrated lenses therapeutic contact for treating dry eye. Once set, these lenses need to be continually re-hydrated with artificial tears.
- Years ago they have also used other techniques now disused or completely forgotten as soft laser therapy and radiotherapy.
Replacement therapy for dry eye with artificial tears
 The replacement therapy with artificial tears and lubricants is currently the most widely used therapy for dry eye. Not only relieves dryness and makes the patient more comfortable, some studies have shown that the use of tear smoothes the surface of the cornea and more regular and can contribute to an improvement in vision.
The replacement therapy with artificial tears and lubricants is currently the most widely used therapy for dry eye. Not only relieves dryness and makes the patient more comfortable, some studies have shown that the use of tear smoothes the surface of the cornea and more regular and can contribute to an improvement in vision.
But this treatment has its limitations: natural tear has a complex composition of water, salts, hydrocarbons, proteins and lipids that are very difficult to match with replacement therapy.
Moreover, natural tear secretion is continuous, while the artificial tear is instilled only periodically. To overcome this limitation, are prepared with substances to increase the contact time of the artificial tear with the ocular surface, many formulated as viscous gels, with the disadvantage that can cause blurred vision and deposits on the eyelashes.
In fact, artificial tears must not only reproduce the characteristics of natural tears, but bring new features: should last longer in the lacrimal basin and its composition should include drugs and principles repair primary and secondary lesions dry eye there may be.
A common component of artificial tears are buffers that serve to maintain the natural pH of the tear. This is important since the pH of the tear film must be kept constant to maintain the normal function of the epithelial cells. In addition, the pH decreases after instillation of eye drops more alkaline and quickly done before normalize in about 2 minutes. The addition of buffers to tears is done to bring about this change more slowly.
A disadvantage of many of the artificial tears is that they include preservatives, stabilizers and other additives. These substances are often cause worsening of the disease, so the ideal is the use of tears in single dose format, as they lack preservatives. In fact, patients who tears need to be applied over four times daily wear contact lenses have ocular surface or lacrimal drainage obstruction disease should use prepared without preservatives.
Aqueous tear pharmacological stimulation for dry eye
This treatment is very useful in patients with Sjögren's syndrome, immune disorder that affects the tear-producing glands and saliva. Even when the disease is well advanced it might not be a good therapeutic alternative.
The only substances capable of increasing tear production are parasympathomimetic, pilocarpine and cevimeline especially. Oral pilocarpine increases tear production and improving the symptoms of dry eye, reaches a maximum at 10 minutes and persisted at 30 minutes. Regarding side effects, also it acts on receptors cardiac M2, and may stimulate airway smooth muscle and bowel, contracting it also causes sweating, headache and nausea. However, these side effects are usually well tolerated.
- The dose considered optimum is 20 mg / day and the drug loses lower doses lacrimal effectiveness, while maintaining the salivary. Treatment should begin gradually: 5 mg / day in the first week, 10 mg / day the second week, 15 mg / day and 20 mg third / fourth day, thus the adverse effects will be lower. It is contraindicated in patients with severe COPD, severe kidney disease and heart disease.
Treatment of dry eye with mucosecretores and mucolytics
Bromhexine orally at doses 24-48 mg daily in 3 doses, it seems to improve mucus secretions, as well as some authors observed acuoserosa also improves tear secretion.
N-acetylcysteine is a mucolytic, stimulating and facilitating the production of mucin which is administered orally at doses of 300 mg daily in 3 doses. The mucous layer of the tear is usually altered in patients with dry eye. This can be very viscous and form plaques and filaments on the ocular surface causing irritation and pain, so the application of mucolytic solutions can be very useful.
Pentosan polysulfate sodium is an anticoagulant with mucorreguladora action, which has been used in mucodeficientes cystitis, and has also shown efficacy in dry eye.
Occlusion of the drainage system Dry Eye
Occlusion of the canaliculi and puncta prevents tear drainage: the most widely used non - pharmacological treatment for dry eye.
This technique improves the quantity and quality of the aqueous component, improving dry eye symptoms and reducing the frequency of administration with artificial tears are needed.
There are some possible complications, such as rupture punctal, pruritus, suppurative canaliculitis canalicular stenosis, and silicone plugs used to occlude described pyogenic granulomas.
This treatment is usually reserved for severe cases of dry eye, when the frequent use of artificial tears without preservatives is not enough, especially in the types of aqueous deficit.
Occlusion procedures commonly used punctum are:
- Surgical: They are not widely used because of its difficulty to reverse them , with the exception of punctal patch technique.
- Thermal: Produce closure canalículo to destroy and retract your wall. To do this you can use cautery, diathermy or argon laser. The former has the disadvantage that a high percentage of cases is recanalizes canaliculus and also burns produced can distort the eyelid. Argon laser allows partial or total blockages and punctal openings.
- Tamponade methods: They are the most used, and consist occlude the drainage path through the introduction of a foreign body, a resorbable or non - resorbable implant. They are the most common because it does not require surgery and can easily be reversed.
Non-resorbable implants are divided into:
- Punctal plugs, which can be silicone or teflon HEMA. The head of the cap is hovering outside the canalículo, so it can irritate the conjunctiva and cornea. Other possible complications include itching, suppurative canaliculitis, intrusion, fragmentation of the plug and canalicular stenosis by local irritation.
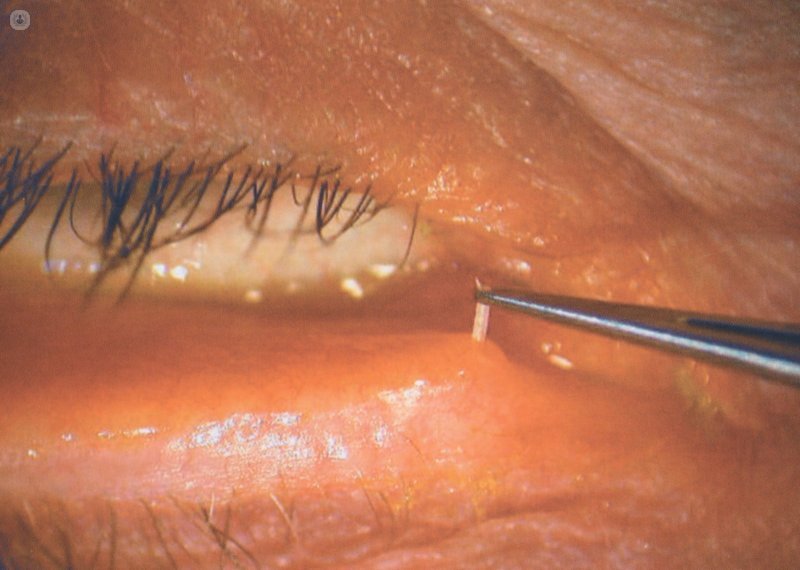
 Placing a punctal plug nonabsorbable
Placing a punctal plug nonabsorbable - Canalicular plugs, which are inserted silicone and past the punctum into the horizontal portion of the canaliculus, so as not poke through punctal not irritate the eye.
Resorbable implants for the treatment of dry eye can be made of hydroxypropyl cellulose, material causes release slowly with body temperature, collagen, that only partially reduce the flow canalicular 60-80% or catgut. This method of plugging is chosen, it not only allows clinical improvement in patients, but also allows treating dry eye temporarily.
 Punctal occlusion with resorbable collagen plug
Punctal occlusion with resorbable collagen plug
Surgery to treat Dry Eye
Surgical solutions for dry eye are manifold, as blefarorrafia, blepharoptosis, lacrimocitos transplants, cisternoplastia, transposition of parotid duct, salivary gland transplants, etc.. In addition, there are also surgeries that treat diseases that cause or worsen dry eye, such as conjuntivochalasia or floppy, among others.
Alternative Treatments for Dry Eye
Topical Vitamin A: It is essential for normal epithelial growth and its deficiency can cause dry eye, even in severe cases keratinization. Although derivatives topical vitamin A are capable of reversing squamous metaplasia and keratinization of the ocular surface, this occurs only in severe cases of dry eye because in most moderate dry eyes not these changes are given in ocular surface.
Autologous serum topic: It has been shown that use 20% diluted in saline for four weeks improves test results of rose bengal staining and fluorescein in dry eye patients. It is indicated especially in patients with severe disease and persistent epithelial defects.
Topical cyclosporine due to the inflammatory nature of dry eye, at least in part, their use as anti - inflammatory and immunomodulatory improves dry eye cases also linked to Sjogren syndrome.
Polyunsaturated fatty acids orally: has been attributed improvement in dry eye after supplementation with essential fatty acids Omega 3 DHA (docosahexaenoic acid) and GLA (gamma - linolenic acid) because of the change in the glandular phospholipid composition and its product excretion, the increase in the amount and thickness of the lipid film and pacing stimulation of prostaglandin E1 to activate glandular secretion lacrimal. Also in cases of treatment with polyunsaturated fatty acids prior to LASIK surgery have risen figures lactoferrin in tears, a diagnostic marker of eye health.


