Anterior cruciate ligament injuries of the knee: intervention and rehabilitation
Written by: The ligaments of the knee allow to maintain its stability, attaching it to the femur and the tibia. The ACL intervention is usually done by arthroscopy, replacing the anterior cruciate ligament with a new one. In all cases of young people the operation is recommended, since 80% of patients with broken and non-operated ligaments have degenerative signs, as well as meniscal and cartilaginous lesions. 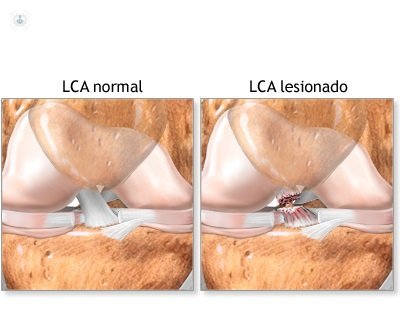
Anterior cruciate ligament of the knee: what is
The knee has four fundamental ligaments that are:
- Anterior Cruciate Ligament (ACL)
- Posterior Cruciate Ligament (LCP)
- Inner Lateral Ligament (LLI)
- External Lateral Ligament (LLE)
The knee joint communicates in its upper part the femur and in the lower tibia. If it were not for the ligaments, the femur and the tibia would move with respect to one another and the stability of the knee would not be maintained.Only the ACL and the LCP are inside the joint and, therefore, can be operated by arthroscopy. In contrast, lesions of LLI and LLE can only be operated in a traditional way, with open surgery.
ACL, essential for knee stability
As the name suggests, the lateral ligaments are on the sides of the knee and go from the femur to the tibia, each on its corresponding side.
The cruciate ligaments intersect with each other forming a kind of X inside the knee: one of them is overlapped in the front (anterior cruciate ligament) and the other crosses behind (posterior cruciate ligament). As an example, the ACL is a "rope" that prevents the tibia from moving forward; while the LCP crosses behind and prevents the tibia from moving backwards.
The most frequent lesions are LLI because a valgus injury is more likely to occur, from the knee inwards and standing out, with elongation or rupture of this ligament.When there is a rupture of one of these structures in an athlete, being a young patient with biomechanical requirements and stability of 100% for their sporting activity, the surgical indication is practically unavoidable. When it comes to an injury that is not an athlete, a reasonable doubt arises:
1) Should I operate?
The clinic is the one that "commands". That is, if your knee is unstable it is convenient to operate. In older than 45 years the indication must be qualified according to the degree of physical activity or the profession. Those who do not operate should know that the ACL does not "self-repair", that they should decrease their physical activity (avoid contact sports, changes of direction and rotation in their knee.) And, in case of any clinical manifestation of instability, they should to operate. In addition, 80% of patients with ruptured and non-operated cruciate ligaments have significant degenerative signs with meniscal and cartilaginous lesions.
Once the replacement surgery is decided, other questions arise:
2) When do I operate?
There is no consensus, but much scientific evidence suggests that surgical intervention is desirable when inflammation has subsided and the knee mobility arch is complete, a situation that usually occurs after the third week of the accident.
3) What is the operation?
All the intervention is performed by arthroscopy, with the injured conscious and seeing the intervention in a monitor. The patient will leave the hospital on his own. In surgery, the broken ACL is replaced by a new ACL, which is "made" with tendons that can be:
- Autologists: they are the patient's own.
- Allograft: they come from another person, usually from a corpse.
- Synthetic or animal grafts were used, but they are in disuse.
Factors that influence the success or otherwise of the ACL operation
Either of the two previously described options has advantages and disadvantages. The use of one or the other will depend on the individual characteristics of the injured, the experience of the surgeon and the availability of grafts in the tissue banks. This is because, depending on whether we choose a graft or another, there will be a greater or lesser risk of suffering a poor result, postoperative discomfort of the donor site, infection, biocompatibility, the process will be more or less expensive and more or less durable. The advice is to rely on the criteria of your specialist knee traumatologist , as it will offer the best option, whether indicated or not, as the technique to be performed and the graft to be placed.
Recovery of Anterior Cruciate Ligament Surgery
Although this surgery is currently performed by arthroscopy , it must be taken into account that the surgeon works within a joint without being able to avoid manipulating its components (bone, cartilage, etc.). For this reason, it takes time for the knee to retrain and the replacement plasty to be integrated. Thus, at three months nerve endings are formed and at six months functional levels similar to those prior to ACL rupture are achieved. Even so, it should be noted that until the year is not fulfilled, plasticity does not behave like the "ideal" LCA. Knowing this allows us to schedule rehabilitation therapy.
The patient has to assume that the incorporation into everyday activities and sports is progressive and slow. In addition, their "role" during rehabilitation is fundamental. All your effort should focus on achieving the following objectives:- Recover full mobility- Get Muscle Power- Gain stability of the knee joint
Rehabilitation should begin weeks before surgery so that the musculo-osteotendinous structures are in their best physical condition.
Early mobilization of the joint after ACL reconstruction can reduce pain, decrease adverse changes in articular cartilage, promote joint nutrition, promote healing, and prevent joint capsule contraction.Patients with delayed lenses, who do not reach full extension and / or flexion by 90 degrees in two weeks, should be treated more aggressively, ie applying manual pressure or forced stretching.
Of course the postoperative recovery will be in the hands of the rehabilitator and physiotherapist specialized in knee pathology.
.