Dry eye diagnostic tests
Written by:Dry eye or keratoconjunctivitis sicca (KCS) is the name that describes several clinical diseases Ophthalmology ; all preocular tear altering film, which causes a disease of the ocular surface are altered by which the volume of tears, the composition thereof and hydrodynamic factors.
Dry eye symptoms
Dry eye is a disease that the patient does not go unnoticed. Symptoms usually clear and unpleasantly common:
- Feeling of "sand in the eyes"
- dry eyes
- Intolerance to contact lenses for the same dryness
- Fluctuations in vision that lasts until one or more flickers recover an optimally suitable for viewing tear film
- Epiphora, ie, abundant and constant watering
- Burning eyes
- Itching, tingling or skin irritation of the eyes
- Photophobia
The presentation of these symptoms is highly variable. Precisely one of the characteristics of dry eye is that of the day and night differences in the incidence of symptoms. For example, aqueous secretion is greatly reduced and minimized at dusk during nighttime sleep, which, together with the common hypoxia during this period with closed eyes is accompanied by a significant increase in symptoms upon awakening.
Diagnosis of dry eye
The correct diagnosis of the disease is what best we can lead the most appropriate treatment. There are several methods of study and objectives diagnostic tests are used clinically to measure the integrity and stability of the tear film preocular. However, today there is no evidence that alone can diagnose all types of dry eye. What is needed is to have a diagnosis that provides knowledge of the degree of severity, the affected subsystem and origin in order to develop a more specific treatment accordingly.
Existing diagnostic tests ophthalmology are currently the following:
anamnesis
The anamnesis is a verbal exploration, in which the ophthalmologist should hear the description that the patient makes his illness, and simultaneously help you remember situations and symptoms spontaneously does not count because it does not relate to their disease. You need to know the symptoms, when they started, how they evolved, how they have been treated and in what situations better and worse.
Are also of great interest especially family and personal history, habits and workplace and home of the patient, not to mention taking treatments for other reasons as some or several of them can cause or exacerbate dry eye.
exploratory findings
Within the semiotics of dry eye we can distinguish between Biomicroscopical findings or detected with the slit lamp and those seen with the naked eye as would be the following:
- Dullness in his eyes and look sad.
- repetitive wiping of the eyes or touching them frequently.
- Increased blink rate and in some cases blepharospasm.
- periquerática querática and conjunctival congestion.
- Inflammation of the eyelid margins, excess tear feeling in them, etc.
And, after observing the ocular surface and the skin around the eyes, finally they should also look at other aspects such as: the skin of the face for acne rosacea, seborrheic dermatitis, etc .; feel the parotid glands, submaxillary and submandibular; examine the mouth by saliva; hands look for signs of joint inflammation; petechial rashes and eczema, etc.
Tests for quantitative and qualitative analysis of the tear
Schirmer Test: This test devised Schirmer in 1903 and involves placing a strip of filter paper in the eye socket. The patient should normally flash for 5 minutes, sitting in the cabinet exploration, which should be no bright lights or air currents. After 5 minutes the strip is removed and the wet linear millimeters are recorded on the strip portion not inserted behind the eyelid. Thus it is considered normal value greater than 15 mm, and a result less than 5.5 mm is considered diagnostic of aqueous tear deficiency.
Testing the basal secretion Jones: Later, in 1966, Jones proposed to test after applying anesthetic, in order to quantify the "basal" tear production, as opposed to production "reflects" that would measure the Schirmer test I. In this case it is considered a figure of less than 10 mm is pathological.
Test tear clearance: Despite the limitations in its implementation, it should be noted that this test has a higher correlation than Schirmer with symptoms of eye irritation and is more common with older age, meibomian disease and decreased sensitivity corneal-conjunctival .
Other tests or laboratory: There is evidence that require more sophistication to its implementation and would in this section:
- Study Osmolarity
- Proteinogram (by electrophoresis)
- Crystallization tests of the aqueous layer of the tear film
Analysis of the stability of the film
Tear breakup time: This test is performed by applying a drop of fluorescein in the eye, and quantifying the appearance of a black spot after the last flicker. Often the test should be repeated more than once, to avoid environmental factors such as heat or drafts. It is considered normal that ink remains in the eye between 10 and 15 seconds, and if given a lower value, will be indicative of poor tear quality, but no clinical difference type of dry eye.

Fluorescein in one eye during the analysis of tear break
Analysis of ocular surface
Fluorescein staining: fluorescein instillation or 1-2% by strips of paper, allows the specialist ophthalmologist observed in few seconds corneal areas where the absence of epithelium. Also, fluorescein allows better visualization of the size of the tear meniscus and mucous filaments. For display is required cobalt blue light.
Rose bengal rose bengal dye accommodates devitalized cells and keratinization phase, and which are not covered by mucin. Staining is evaluated without the blue light, the mucin secretion and filaments are also tinged with rose bengal. Therefore the use of fluorescein and rose allows objectify epithelial damage and the state of the mucin layer. This dye causes intense itching, even more marked in dry eyes.
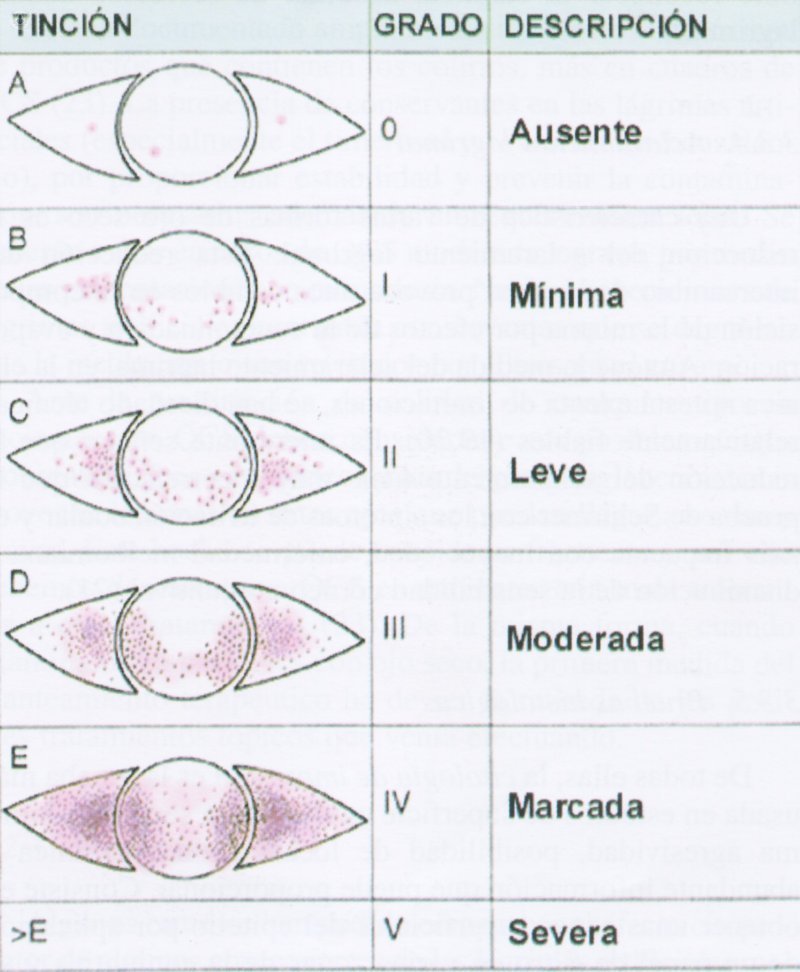
Classification according to degree of injury or rose bengal staining
Green lissamine: To reduce the intense itching caused by the rose bengal, has been proposed green lissamine 1%, with similar properties but with better tolerance and lower toxicity.
histological evidence
Cytology print: all histological evidence of impression cytology is the most used by simplicity, minimal invasiveness, possibility of anatomical location and wealth of information that can provide. It consists obtain superficial epithelial layers by applying a filter paper in various parts of the eye and its study.
Other tests used would be less conjunctival biopsy which provides good information of the disease at the cellular level. And the lip and the salivary glands that may be needed to confirm the diagnosis of Sjögren's syndrome biopsy, although this is not indicated routinely.
Hematological analysis of dry eye
His main interest is in patients with Sjögren's syndrome, which is an autoimmune disease that affects the exocrine glands and leads them to dryness. These analyzes can be found anemia, leucopenia, relative lymphocytosis, eosinophilia, thrombocytosis, thrombocytopenia, increased erythrocyte sedimentation or hipercreatininemia among many other related conditions.
Diagnostic criteria in dry eye
Despite all evidence existing diagnostic, already described, other studies argue that an analysis of symptoms without more is not enough for a differential diagnosis because these symptoms are often present in patients with various types of dry eye.
In short and as a final conclusion, despite the existence of multiple testing and tests (which is why there are so many different), for the diagnosis of dry eye, most effective, important and truly effective is the realization of a good history and examination by an ophthalmologist experienced in the office or medical office.


