Transcranial Magnetic Stimulation to treat neurological diseases
Written by:Transcranial Magnetic Stimulation (EMT) is based on electromagnetic induction to activate cortical neurons, stimulating the cerebral cortex. Assessing the excitability of the cortex will diagnose and estimate the therapeutic application of the technique for diseases such as depression, dystonias, Parkinson's, Cerebrovascular Accidents or epilepsy.
Transcranial magnetic stimulation: what it is and what it consists of
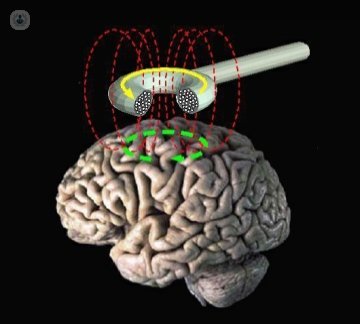
Transcranial Magnetic Stimulation (EMT) uses electromagnetic induction to activate cortical neurons. The stimulator is a capacitor that is discharged by a coil and produces a magnetic field. This, applied through the scalp, in turn induces an electric field. It is a non-invasive method to electrically stimulate the cerebral cortex and to assess the excitability of the motor cortex and the corticospinal tract.
It can be applied by single pulses or by trains of stimuli at variable frequencies. Unique stimuli can depolarize neurons and produce measurable effects. Stimulus trains can modify the cortical excitability of the stimulated zone and related remote areas through anatomical functional connections and their therapeutic application is being investigated.
In 1985, Barkers and colleagues designed an electromagnetic stimulator to stimulate, for the first time, the motor cortex through the scalp.
This stimulation technique, unlike electric stimulation, is painless and non-invasive.
Utilities of transcranial magnetic stimulation and diseases that treats
There are two basic fields of application of transcranial magnetic stimulation: diagnostic and therapeutic. From the point of view of its diagnostic utility it is interested in:
a) Evaluation of the spinal conduction time. It is the time of conduction from the motor cortex to the alpha spinal motoneurons. It consists of the difference between the time of conduction from the cortex to the muscle and the time of conduction peripheral motor. Its fundamental application is used in the diagnosis of myelopathies secondary to discal pathology, canal stenosis or scoliosis, among others. It can also be altered in other pathologies, such as Amyotrophic Lateral Sclerosis or Multiple Sclerosis.
b) Evaluation of excitability of the motor cortex, by determining the motor threshold and period of silence, which can be altered in certain pathologies affecting the central nervous system.
c) Transcranial magnetic stimulation and neurosurgery. TMS can be used for preoperative assessment of specific areas of the brain.
The findings obtained so far may help to locate the level of the lesion along the different motor system levels, distinguishing between a predominantly demyelinating or axonal lesion, or predicting the motor functional outcome after an injury. Anomalies shown by TMS are not disease specific and the results should be interpreted in context with other clinical data.
From the point of view of its therapeutic application, the application of stimulus trains by repetitive Transcranial Magnetic Stimulation has special interest in the treatment of depression. It involves applying a train of EMT pulses of the same intensity in a certain area of the brain and a frequency that can vary from one to 20 stimuli per second. Other possible indications are dystonias, Parkinson's disease, recovery from stroke (CVA) and even treatment of refractory epilepsy.
Preparation Before Transcranial Magnetic Stimulation
In principle it is an innocuous exploration and does not require any preparation except the usual neurophysiological explorations, such as cleaning and absence of creams in the areas of stimulation and registration. However, the previous explanation by the expert in clinical neurophysiology is desirable, to reduce the patient's initial anxiety, and even to try to lower intensities.
Possible Risks of Transcranial Magnetic Stimulation for the Patient's Brain and Contraindications
The adverse effects after a single pulse EMT on the motor cortex are very strange. The potentially adverse effect that has caused most concern so far has been epilepsy, although the risk is remote.
However, there are contraindications to treatment with EMT. In this sense, they are absolute contraindications:
- intracerebral metal material (aneurysm clips)pacemaker- should be questioned about any implanted biomedical device- precaution with cochlear implants
Relative contraindications are:
- Extensive strokes (strokes)- TBI (traumatic brain injury)- history of neurosurgery- family history of epilepsysleep deprivation- pregnancy (in this case the magnetic stimulation at the cortical level does not affect, although it should be avoided at the lumbar level.
Side effects or sensations after treatment with EMT
The most common side effect is headache, mainly due to repeated muscle stimulation. It usually begins at 20-30 minutes after transcranial magnetic stimulation and responds well to regular analgesics. Finally there is a certain risk of secondary transient hearing loss and tinnitus, which is why the earplugs or earplugs are usually used.


